The Ontario Healthcare Crisis
This article is based on a chapter in the upcoming new book Against the People: How Ford Nation is Dismantling Ontario edited by Bryan Evans and Carlo Fanelli. The book will be launched February 18, 2025, 7:00pm, Centre for Social Innovation, 720 Bathurst Street, Toronto. Register here.
Ontario is experiencing unprecedented hospital capacity problems in recent years. Thousands of unplanned closures of hospital emergency departments, permanent closures of some hospital facilities, unprecedented levels of inpatients being treated in hallways, long waits to gain admission into hospitals, and high bed occupancy levels are just some of the key problems undermining Ontario hospitals.
This brief will explain key issues driving these problems and show that the government’s current capacity plan will make the situation worse.
Hospital Bed Capacity
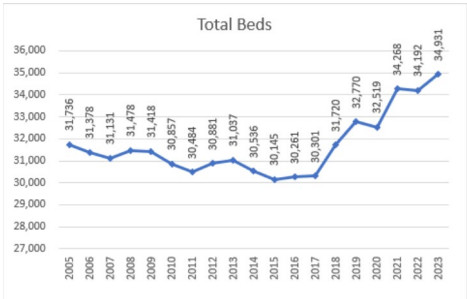
Ontario has a very low number of staffed hospital beds. In 2023, there was 34,931 hospital beds staffed and in operation in Ontario. That is 2.23 beds per 1000 people.1 Despite promises to end hallway healthcare, this is virtually identical to the level when the Progressive Conservative (PC) government came to power in 2018, when there was 31,720 beds and a ratio of 2.21 beds per 1000 population.
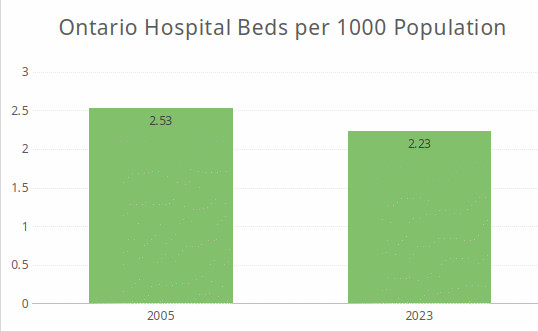
Between 2005 and 2023, hospital beds in Ontario increased from 31,736 to 34,931, a 10% increase. However, population increased 24.6%. As a result, hospital beds per 1000 people decreased from 2.53 to 2.23, a 12% decrease.
To return Ontario to the same capacity relative to population as in 2005, another 4,699 extra hospital beds would have been required in 2023.

This extra 4,699 beds would not account for the extra need created by societal aging. During that same period (2005-2023), the 65 and older population increased by 1.25 million, or by 77.5%.2 As will be discussed below, this also requires a significant increase in hospital capacity – not a decrease.
The Ontario number of beds per 1000 population compares poorly with the rest of Canada – 2.23 versus 2.59.3 The rest of Canada has 16.1% more beds per capita than Ontario.
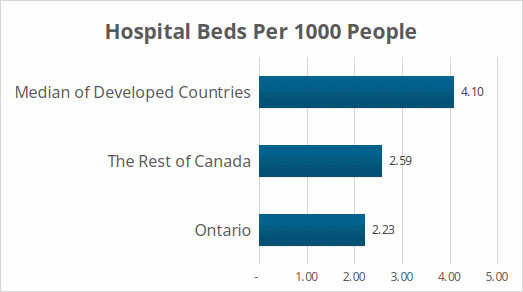
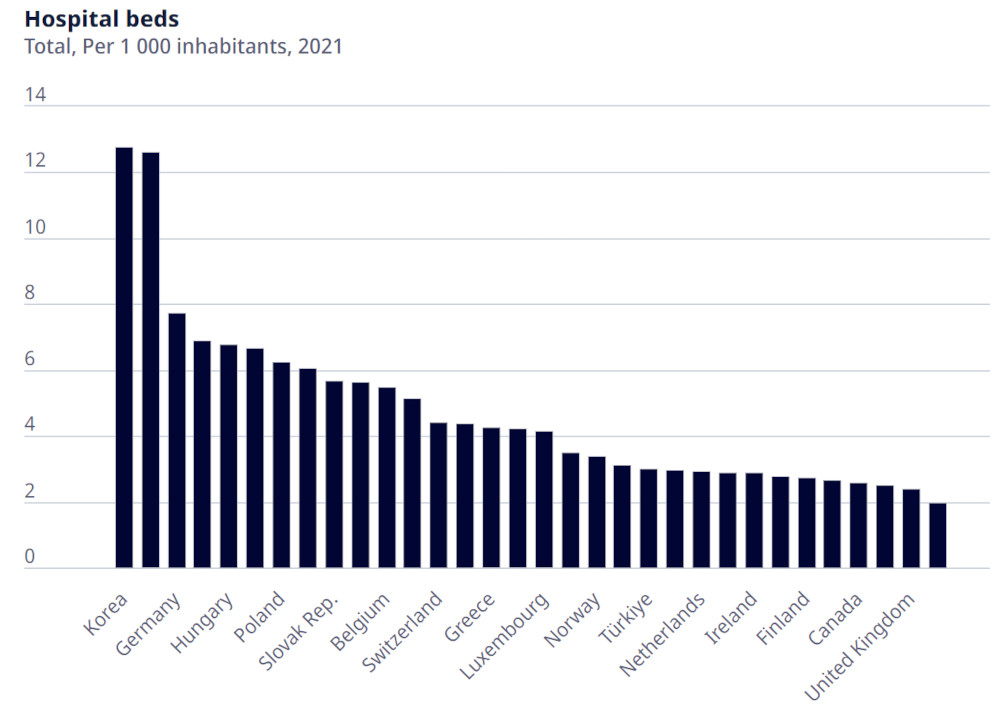
Internationally Ontario is an outlier – only Sweden has fewer hospital beds per capita. The median among rich nations is 4.1 hospital beds per 1,000 population. That is 84% more than Ontario.
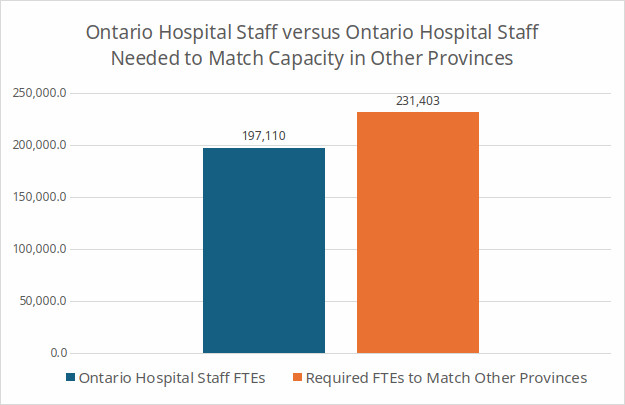
Hospital Staffing: Ontario hospitals drastically understaffed – if we had the same level of staffing as in other provinces, we would have an additional 34,292 extra full-time staff (FTEs).4
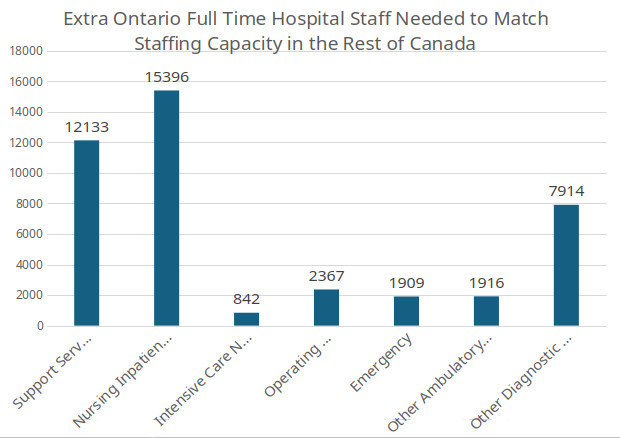
Ontario has low levels of staff in key areas: 12,133 full-time staff are missing in support services (cleaning, food maintenance, etc.), 842 in Intensive Care, 2,367 in operating rooms, 1,909 in Emergency Departments, and fully 15,396 in nursing inpatient services.5
The overall 34,292 FTE staffing shortfall in Ontario occurs despite higher hospital staffing levels in Ontario in non-traditional hospital employment – i.e., research, education and community health.
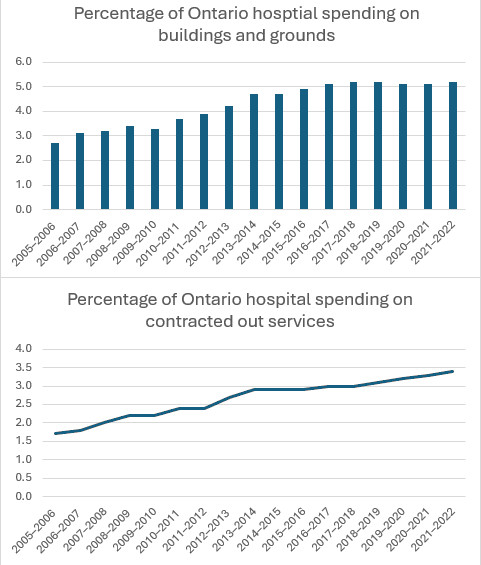
Spending on compensation has decreased as a share of total hospital spending markedly – from 64% to 59%. This decrease in spending on employment coincided with an increase in spending on contracting out and on hospital buildings after the previous provincial PC government turned to much more expensive privatized P3 (Public Private Partnership) hospital facilities starting in the first decade of this century.
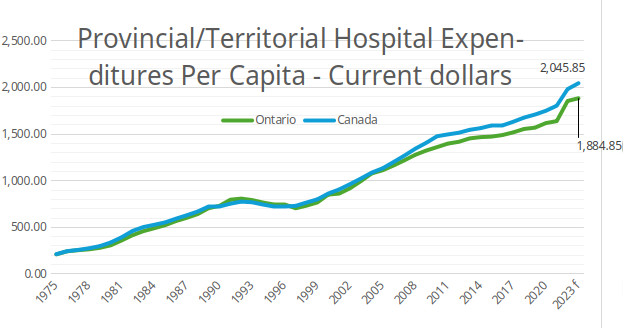
Hospital and Healthcare Funding: Provincial government funding of hospitals is lower in Ontario than any other province, according to the data from the Canadian Institute for Health Information.6
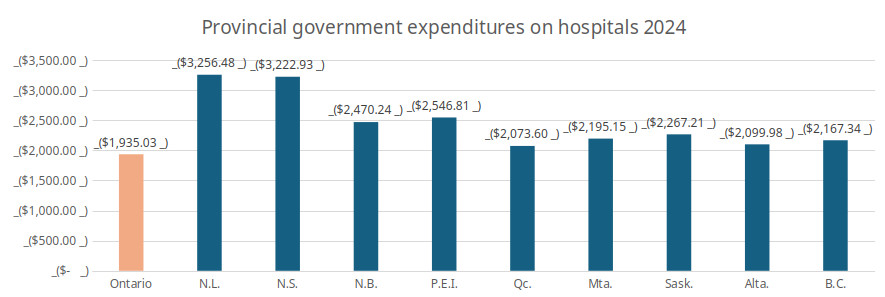
For many decades Ontario followed the Canada-wide funding pattern, but, starting in the first decade of this century, Ontario began to fall behind. According to the latest figures from CIHI, we are about 6.7% behind the Canada-wide average for provincial health expenditures per capita (which, of course, is itself pulled down by Ontario).7
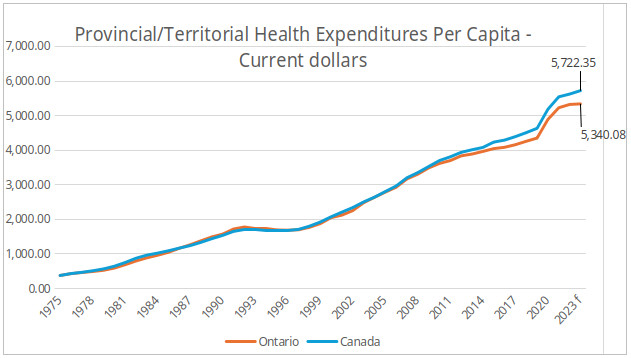
Much of this is due to hospital underfunding, where Ontario is 7.9% behind the Canada-wide average.
The Budget plan was to decrease total provincial hospital funding for 2024/25 by $250-million, almost one percent. However, the Fall Economic Statement (FES) noted a one billion healthcare funding increase. While the FES did not reveal how this would be spent, the Financial Accountability Office indicated that health spending was 6.7% over budget ($2.6-billion) in the first half of the fiscal year and that this included $1.3-billion for hospitals and home care.
This mimics what occurred in 2023/24 where hospital funding was budgeted to increase 0.5% but, largely through an increase announced at the very end of the fiscal year (in the 2024/25 Budget in fact) the total planned increase was much higher (11%).
This is not the way to fund hospitals. It does not allow hospitals to plan appropriate staffing levels and encourages reliance on overtime and much more expensive for-profit staffing agencies. Hospitals need better funding, but they also need clear guidance on hospital funding when the fiscal year begins at the very latest.
By 2023/24 many hospitals were reporting significant deficits – deficits which they have to get special permission from government to run.
Now, it is not clear that the government will 100% fund the need created by the failure of their Bill 124 real wage cuts. The government has chosen to parcel this money out very slowly, if at all. As a result, by the middle of this fiscal year (2024-25) hospitals faced huge working capital problems, large deficits, negative operating margins, high long-term debt, and extremely high bed occupancy. This is no way to run a vital service that saves people’s lives.
The Situation Under the Current Government and Its Future Plans
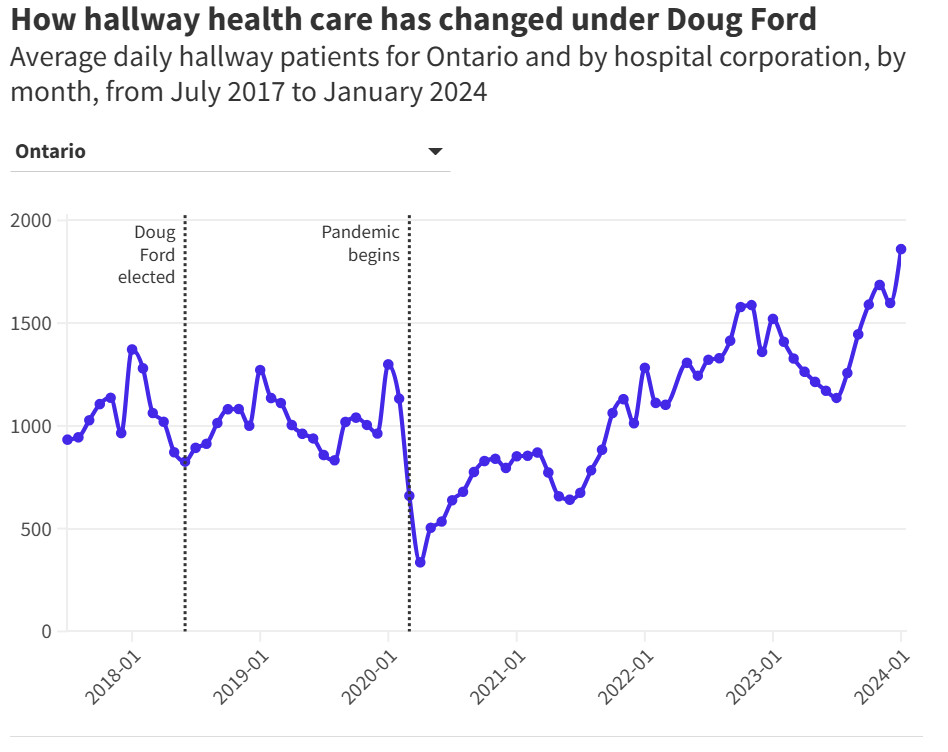
The PC government promised to end hallway healthcare. This promise is now more or less forgotten given the many hospital capacity failures that have arisen during this government’s reign. However, the government does make some promises to increase capacity. These promises do mark a change in policy. After decades of stagnating capacity, the promise now is to increase it. The problem is that what has been done, and what has been promised for the future are totally inadequate to meet the need for care.
The government’s promise to increase LTC capacity remains officially in place – but the government’s execution of this promise has been inept, inadequate, and slow.
A. Hospitals: The government has claimed for some years now that it increased hospital capacity during COVID by 3,000 beds. It further promises that it will increase hospital capacity by another 3,000 beds 2032. If true this would be a capacity increase by almost 18.3% over 13 years, or by about 1.3% per year. There are several problems with this, however.
First, the hospitals themselves report an increase of only 2,161 beds since the COVID pandemic (i.e. since 2019).8
If 3,000 additional beds are added to these figures, this would mean an increase of 15.7%, not 18.3%, or an annual average increase of only 1.1%, not 1.3%.
Second, the demand pressure for hospital and other healthcare capacity is growing much more quickly than 1.1% (or, for that matter, 1.3%) per year.
B. Demand Pressures
1. Population growth: Part of the failure of the government to solve hospital capacity problems lies with their unwillingness to keep up with population growth.
According to Statistics Canada, Ontario’s population in the second quarter of 2018 (when the Ford government was elected) was 14,251,136. This rose to 15,996,989 by the second quarter of 2024, a 12.3% increase. This is a compounded annual average increase of 1.94%.
This puts significantly more pressure on our hospital and healthcare system. Just to keep up with population growth we would have had to have added 12.3% capacity since the Ford government was elected in 2018.
This increase in healthcare demand pressure is exclusive of other health care demand pressures such as aging and increased utilization of healthcare. These other factors, beyond population growth, makes the bed crisis worse. Hospital capacity must go up for reasons aside from population growth.
2. Societal aging. Healthcare needs are very sensitive to aging. Currently about 60% of hospital beds are occupied by people aged 65 or older. This group, however, is growing at a very rapid pace. Between 2018 (when the Ford government was elected) and 2023, the 65+ population has grown 18.4%, or, on average 3.4% per year. To maintain a comparable level hospital bed capacity for this age group, the total number of beds would have to increase by 2.04% each year.9 This level of growth in the elderly population is expected to continue through this decade.
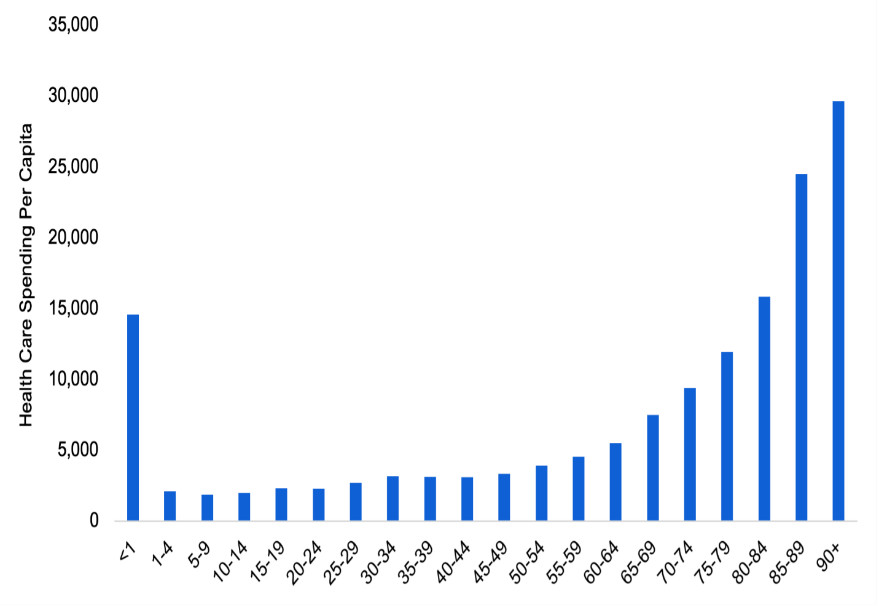
3. Increasing Utilization: Utilization refers to increases in demand for health services that arise outside of population growth and aging. For example, a new medical discovery could result in an increase in utilization. Diseases and conditions that could not be treated, now can be. The last Ministry of Finance in depth discussion of the impact of healthcare utilization estimated that healthcare utilization increases at a constant annual rate of 1.5 per cent.
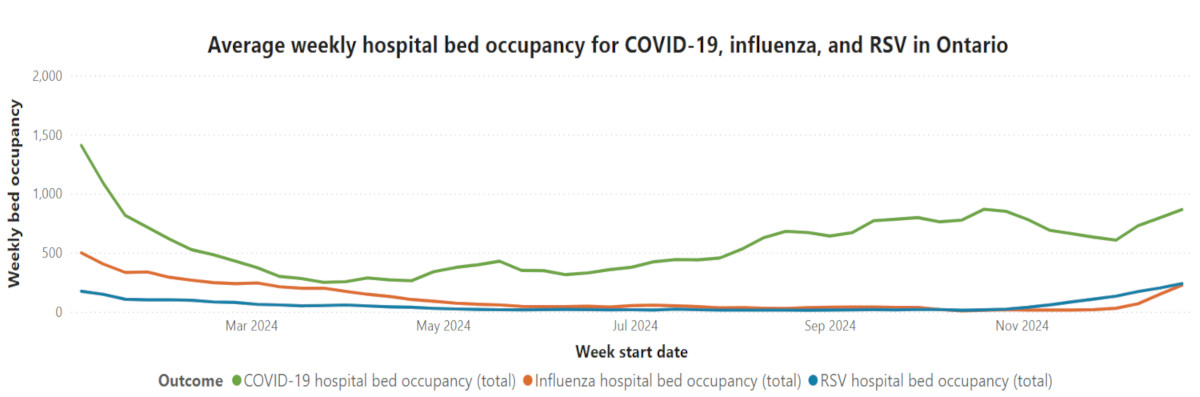
One new factor affecting utilization is COVID. The ultimate impact of COVID and post COVID on hospital demand remains uncertain but right now COVID remains a significant factor affecting hospitalization. Hospitalizations for patients with COVID continued to go up and down over the last year reported (January 7, 2024 through December 22, 2024), ranging from a high of 1,408 on January 7 2024 to a low of 249 on March 24. In the latest report (for December 22, 2024) there was 865. Average weekly COVID bed occupancy remained far above that for influenza or RSV, even during the flu season. Influenza is often associated with hospital bed capacity issues. Notably, CIHI data indicates patients with COVID stay three times as long and cost three times as much as other inpatients.
The health system is also impacted after people no longer have the COVID infection. The exact impact on hospital usage for health conditions affected by post COVID remains unclear. But the Lancet notes in a recent article that post-COVID “can affect multiple organ systems and lead to severe and protracted impairment of function as a result of organ damage. The burden of this disease, both on the individual and on health systems and national economies, is high.”10
At current utilization levels, the growth of the 65+ population is creating annual average increases in demand pressure for hospital services of 2.04% (3.4% x .6). The growth of the under 65 population (averaging 1.336% annually between 2018 and 2023) has created another 0.53% annual increased demand for hospital services. Increasing utilization would add another 1.5%, for a total estimated demand pressure of just over 4%.
Combined, current population growth, aging, and increasing utilization create significant pressure for growth – over 4% per year. That is well over the 1.1% to 1.3% annual increase in hospital bed capacity since the current government was elected and, as we shall see, is over four times the planned hospital bed growth rate over the next ten years. This helps explain the deepening problems faced by our hospital system.
It is important to note that 4% increases would not deal with the staffing crisis, the workload crisis, the bed shortages, the ER back-ups, and it does not offset inflationary cost pressures. This is simply to maintain the current service levels.
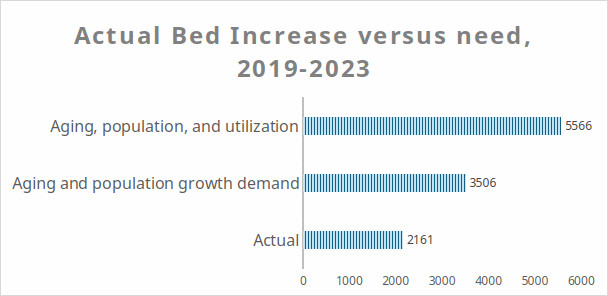
The Future: The existing PC plans for the future are even worse. The official government plan to increase hospital capacity by another 3,000 beds over ten years (approximately 8.6% in total or 0.8% per year) falls even further behind demand pressures – it is less than a quarter of expected demand pressures. Based on population growth and aging, we need 10,095 added beds. Based on population growth, aging and utilization, we need 16,802. We are already thousands of beds behind the capacity we had in 2005. Unless the current PC plan is improved, the decline of the hospital system will intensify.
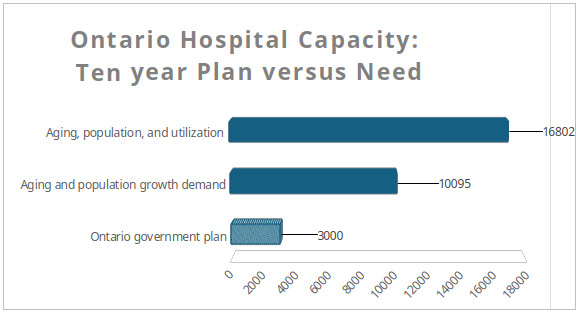
Worse still, a 2023 Financial Accountability Office report indicates that, based on government plans, few new beds will be added between 2022/23 and 2027/28 – 1.8% over five years or 0.3% annually. This is far, far short of what is needed, less than a tenth of need.
Hospital care has been suffering for some years now, but this plan will make it much worse.
Healthcare Infrastructure Failures: The inadequate nature of the government’s actions is found in a multitude of examples. The government frequently boasts about its plans to build new hospitals and LTC beds – but its actions fall far short under examination.
In real dollar terms the Financial Accountability Office reported in 2023 that the ten-year planned increase in health infrastructure funding announced by the provincial government amounts to a 10.8% increase in the actual spend over the previous decade. Meanwhile, the population has grown 18% between 2014 and 2024. That is 2/3 more than the increase in health infrastructure funding. Bed construction is not keeping up with population growth and aging and utilization will more than double the extra demand for health care infrastructure created by population growth.
Long Term Care: The hospital capacity crisis is also compounded by a lack of new long-term care beds. Despite a promise to increase beds by 30,000 by 2028 and by 15,000 by 2023/24, the government reports in the 2024/25 Budget to have only opened 2,246 new beds. That is just 15% of their promise of the number of beds they would create by 2023/24.
In the 2024/25 Fall Economic Statement the government increased its claim, noting that they have added 2,385. That’s an extra 139 beds over seven months. At that rate it will take 125 years to add the 30,000 beds they promised by 2028.
If the 2,385 beds is a net increase in beds, it would amount to a 3.0% increase in the total number of LTC beds. However, the population of the relevant age group (75+) increased by 21% between 2018 and 2023. As with hospital infrastructure, LTC infrastructure development has fallen far short of need – and government promises.
It is unlikely however that there has been a net increase of 2,385 beds, as some LTC operators are closing facilities and beds. In Toronto, six entire LTC facilities have closed or have announced their closure since 2022. This will close 650 beds. Homes in Guelph and Burlington have also announced closures of their facilities.11
The government is having serious difficulties with LTC development. There is no relief coming for the capacity crisis from LTC.
In 2011, Ontario had 90 LTC beds per 1000 elders 75 and older. Indeed, the Health Service Restructuring Commission of the Mike Harris PC government aimed to have a ratio of 96.4 beds per 1000 individuals 75 and older.12 Currently we are at about 61 beds per 1,000 people 75 and older. This is a decline from 74 beds per 1,000 population 75 and older in 2018 when the present government was first elected. This is a 14% decline.
Given the lack of new beds, the wait list for LTC has grown to 48,000, about 33% more than when the PCs were elected in 2018 on a promise of adding many more LTC beds.
The current government’s failure to meet its promises to increase LTC capacity in a timely way contrasts with the previous PC government. It promised in 1998 to add beds and, by 2005, 17,000 new beds had been added.13
Home care: The government trumpets new money for home care – but the Financial Accountability Office projects a decline in the number of nursing and personal support hours per Ontarian aged 65 and over, from 20.6 hours in 2019/20 to 19.4 hours in 2025/26. That is down 5.8% – almost 1% per year. Unless this improves there will be no relief through home care – in fact just the opposite.
Primary Care: The number of Ontario residents who don’t have a family doctor – currently around 2.3 million people – will nearly double in the next two years, the Ontario Medical Association reported in January 2024. This is up from 1.8 million in March 2020. The government responded in the 2024/25 Budget by promising $546-million over three years, claiming this will connect 600,000 people to primary care.
Notably, however, over the last three years, Ontario’s population increased from 14.80 million to 15.99 million, an increase of almost 1.2 million people.
Once again, the government announces impressive sounding numbers that do not stand up under scrutiny.
The consequences of PC policy to date: In 2018, the Progressive Conservatives ran on a promise of ending hospital hallway healthcare. In fact, the problem has gotten worse. The most recent figures put the number of patients at 1,860. This is up by over 1,000 hallway patients compared to when the current government was first elected, i.e. up 125%.
In an unprecedented development, we now have hundreds of unplanned hospital Emergency Department closures every year, often due to staffing problems. Prior to the Ford government this happened only very rarely. Small town and rural hospital are especially under threat.
After the hospital crisis and the cancellation of tens of thousands of surgeries with COVID, hospital bed occupancy fell from 96% in 2018/19 to 84% in 2020/21 – an almost safe bed occupancy level. However, hospital bed occupancy returned to 93% by the first quarter of 202314 and, as of the fall 2024, had increased further to 97.6%, a dangerously high level.
With so few hospital beds and staff, patients who turn up at Emergency Departments must wait. Currently the average wait time is 20.4 hours before a patient can be admitted to the hospital. This is well over twice the target wait time of eight hours. Over the last year reported, only about a quarter of patients admitted to hospital via emergency rooms are admitted within the target time set by the government.
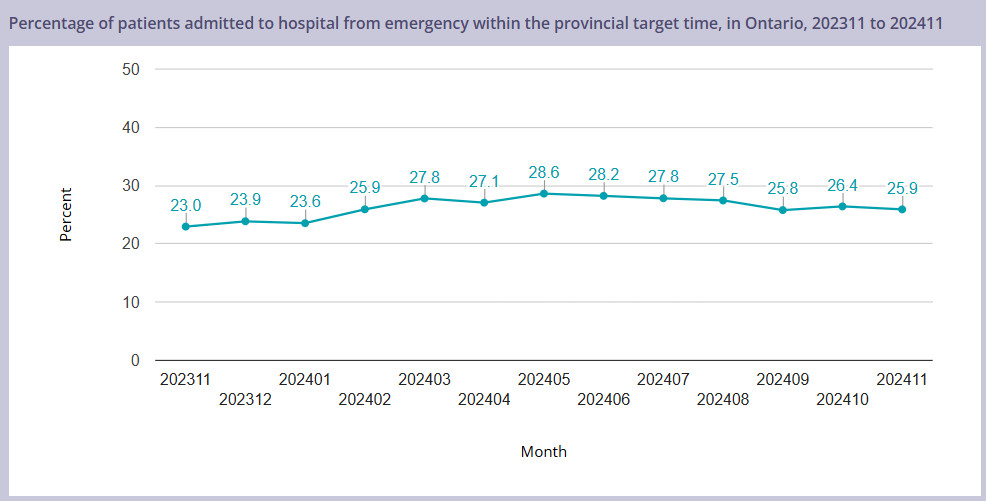
That is a 75% failure rate. This is not because of unusual increases in Emergency Department admissions. In fact, admissions via Emergency Department have been stable over the past year and highly predictable.
The Healthcare Workforce
Exploitation
The healthcare system is sustained by exploiting the compassion of its largely female workforce. Staff work through breaks and lunches, arrive early, and stay late without any claim of overtime. They work extra shifts constantly. Scheduling is blind to its responsibilities for childcare, with 12-hour workdays, rotating shifts, and few weekends off. Vacations and unscheduled days off (for a wedding or a graduation, for example) are hard to obtain given the level of understaffing across all health sub-sectors.
Healthcare workers are denied civil liberties like the rights to strike or to refuse unsafe work. Removing these rights ensures that the workforce is less powerful. During COVID, no work refusals were upheld by the Ministry of Labour of hundreds initiated, including that of a pregnant woman asked to clean a COVID patient’s room without real protective equipment- despite the known risk to mothers and foetus. This worker and many others were forced to do work that was unsafe. Officially, at least 17 Ontario health care staff died, many will never work again.
Casualization
Work is increasingly part-time – 50% of hospital work and 60% of long-term care jobs are part-time or casual. These workers depend on the good will of their supervisors for hours of work and for the quality of their assignments. Full-time employees depend on that good will too, for the quality of their work assignments and for unscheduled time off.
It is less expensive to employ full-time, but employers favour part-time work because it leaves the workers more vulnerable and less resistant to ever-increasing workloads. Increasing part-time staffing has been key to shift from work assignments which were stable and covered absences, to schedules which plan for the absence of several staff on each unit, every shift.
This power over the workforce has delivered quality health care through austerity and downsizing. Health care management compensates for the shortfall in staffing and capacity by guilting and coercing caregivers to treat greater and greater volumes of very sick patients and residents without complaint- despite staff shortages that are ongoing and worsening. Those who speak out about the conditions of work are often harassed, disciplined, and sometimes fired (like a nurse from North Bay who spoke out against violence against staff in our hospitals).
Compensation
Compensation for healthcare workers has been restrained by successive governments using wage rollbacks, limitations on bargaining and provincial wage mandates limiting funding for wage costs to employers. As a result, the income of Ontario health care workers has been cut consistently in real terms.
Bill 124 in Ontario, which limited compensation increases of all kinds to a total of no more than 1% a year for a 3-year period, was introduced shortly before inflation began to soar in Ontario. It coincided with the pandemic, so health care workers who were asked to put their lives and well-being on the line and to work without adequate protection took significant real wage cuts.
Retention Crisis
Ontario is experiencing a retention crisis across health care as the workforce leaves in record numbers, driven by aging, workloads, and the lure of jobs with an equivalent after tax income, sane hours of work and little emotional stress or risk of injury or violence.
Based on the government’s existing capacity plans the Financial Accountability Office a shortage by 2027/28 of 33,000 nurses and personal support workers in Ontario. The FAO also estimates that the total compliment of nurses and PSWs must be expanded by 53,700 by 2027/28.15 Brutal working conditions and low pay mean there will be an especially large shortage of PSWs. Approximately 40% of PSWs leave the health care sector after graduating or within a year of training according to a government report.16
Workloads and Moral Injury
Having the fewest number of hospital staff to patients and the second fewest number of long-term care staff to residents of any province in Canada means workloads are backbreaking and unsustainable. As vacancies grow, workloads increase.
Anxiety, depression, stress, and dread of going to work are feelings reported by most workers in a Nanos poll of Ontario hospital staff. Fueling these emotions is a moral injury caused by the guilt of failing to provide patients with the quality of care that staff know they should provide.
Violence
Healthcare staff face a pandemic of workplace violence. Tens of thousands have been assaulted physically, sexually, racially, or verbally in the last few years. A river of suffering. Polling of hospital workers and long-term care workers in Ontario shows eye-popping levels of assaults of all kinds and a toxic environment for women in these workplaces.
The Globe and Mail ran a powerful series on the violence that women in Canadian society experience. It found that violence is rampant, and that racialized and Indigenous women are particularly vulnerable. The victim is usually blamed. The police rarely press charges. The courts fail most victims.
In a female-dominated, largely racialized working environment like health care society’s attitudes towards violence against women inevitably permeate the institutions. This work is inherently unsafe.
Impact on the people of Ontario
Living with the most under-resourced health care system in Canada (measured by beds to population, staff to population, and over-all spending) has a profound impact on the quality of care available to the people of Ontario. When aging, population growth and utilization are figured in, the capacity of the Ontario health care system is completely strained.
The waiting time for surgeries for many people in Ontario is much longer than is medically recommended; thousands die on wait lists for procedures; people are pushed out of hospital while acutely ill; over 1,300 people a day are on hallway stretchers; people wait months for a long-term care bed; home care is strictly rationed, and many people have no access to primary care.
Solutions
This leads to increasing frustration and a thirst for solutions. Unfortunately, the only solutions offered by the Ford government have been to increase private delivery, including with lucrative subsidies and mark-ups; to provide modest incentives for nurses to work in Ontario; to expand nursing programmes and to continue to underfund the public system.
We believe these could be solutions to our current health care crisis:
- End private sector delivery of acute, long-term care and community health services – it is much more expensive than public delivery and less efficient in terms of quality and mortality. But the lion’s share of new long-term care beds is being given to the private sector to operate. With Bill 60, surgeries like cataracts, and hips, and knees are being privatized, with the province paying three times as much for the service privately provided as it does in public hospitals.
- Capacity must be increased significantly in acute care, complex continuing care, rehabilitation care, mental healthcare, palliative care, long-term care, and home care to meet the needs of an aging and growing population.
- The standards of care in long-term care must be lifted to the four hours of care per resident, legislated but not yet implemented. Bed capacity must also be increased much more quickly.
- The chaos of home care in Ontario must be addressed by returning to public delivery of the service, as envisioned in legislation passed by the Rae government, but never given Royal Assent. Capacity must increase.
- Compensation must be standardized across the health sector, as in British Columbia, to ensure that nurses and other staff in home care and the community sector do not gravitate to work for higher pay in hospitals and long-term care.
- Medical school places and residencies and nursing programs must be significantly expanded. Student physicians, nurses and other scarce professions should receive support for living expenses while studying, in return for agreeing to practice in Ontario.
- The use of nurse practitioners to lead primary care clinics should be significantly expanded.
- Outreach should be made to the thousands of staff who are no longer working, with incentives to recruit them back to work.
- All staff should work to their full scope of practice. This would alleviate some of the current pressures.
- Ban the use of nursing agency staff. These agencies charge two- and three-times what institutions pay their own staff, they bleed away resources from round the clock and weekend staffng, worsen morale and weaken the continuity of care.
- Real wages must increase. In any other labour market with skill shortages, wages would increase to retain and recruit. But real wages are being cut for Ontario’s female healthcare workers and this policy is leading to an exodus of staff and to demoralization.
- Improve nurse morale and retention and significantly improve patient satisfaction and outcomes by moving to nurse-to-patient ratios, as British Columbia has done.
- Increase the percentage of full-time work in the health sector to 70% as recommended by the SARS Commission. Turning part-time work into full-time will increase healthcare capacity and create a more stable and attractive work environment.
- Address violence in healthcare. Adding staff, a culture of zero tolerance, restricting working alone, providing whistle blower protection, prosecuting those who attack healthcare workers are all part of the solution to the problem of violence
Despite problems, brought on by consistent underfunding and by privatization, our healthcare system in Ontario remains a vital social program that must be defended and supported. With help, it can do so much better for the people of this province.
Conclusion:
Ontario lacks hospital capacity, as well as capacity in other key healthcare areas. Under the current government, hospital capacity has fallen behind the growth in need. The government’s plans for the future, especially for the next several years, will see capacity fall behind at an even more rapid pace. The government capacity plan has to improve. •
Endnotes
- Calculated from hospital 2023 bed data and 2023 Statistics Canada population report.
- Statistics Canada. Table 17-10-0005-01 Population estimates on July 1, by age and gender.
- The figures for the rest of Canada are based on the latest Canada-wide data from CIHI data tables, Number of Hospital Beds Staffed and In Operation: Breakdown by care setting, 2021–2022.
- Calculated from Canada Institute for Health Information data on hospital full time equivalent employees (FTEs) by service area, province/territory and Canada (excluding Quebec and Nunavut) 2021/2 and from Statistics Canada second quarter 2021 provincial population reports.
- CIHI, Trends in Hospital Spending, 2009–2010 to 2021–2022 – Data Tables – Series E: Hospital Calculated Full-Time Equivalents by Service Area.
- National Health Expenditure Database, 2023, Canadian Institute for Health Information. Provincial government per capita health expenditure by use of funds in current dollars, Ontario, 1975 to 2023. Nbex Full data tables 2023.
- Canadian Institute for Health Information (CIHI), National Health Expenditure Trends, 2023, Data Tables: Provincial government per capita health expenditure by use of funds in current dollars, Ontario, 1975 to 2023 and Provincial/territorial government health expenditure per capita by use of funds in current dollars, Canada, 1975 to 2023.
- Hospital bed numbers are reported by hospitals in hospital collective bargaining as required by disclosure.
- The actual demand pressures are likely greater as the oldest part of the 65 and older age group (which requires much more healthcare) is growing more rapidly. The 75 and older age group grew 21% over the five-year period – or at an annual average rate of 3.9% since 2018. According to the Ontario Ministry of Finance projections, this more rapid growth of the oldest part of the elderly population is expected to continue.
- Trisha Greenhalgh et. Al, The Lancet, “Long Covid: A clinical update,” July 21, 2024.
- It is notable that LTC operators report only 76,000 available beds as of January 2024 based on government data – a decline in the number of operating beds (78,000 were reported by the government in 2019).
- Ontario Legislature, Standing Committee of Public Accounts, Long-Term Care Facilities Activity. (Section 4.04, 2004 Annual Report of the Provincial Auditor), 2nd Session, 38th Parliament 54 Elizabeth II, 2005.
- Ontario Legislature, Standing Committee of Public Accounts, Long-Term Care Facilities Activity. (Section 4.04, 2004 Annual Report of the Provincial Auditor), 2nd Session, 38th Parliament 54 Elizabeth II, 2005. See pages 2 and 11.
- FAO, Ontario Health Sector: Spending Plan Review, March 2023.
- Financial Accountability Office, Ontario Health Sector, Spending Plan Review, March 8, 2023.
- Ontario, Long-Term Care Staffing Study, July 30, 2020.